Journal Club: Cancer Biology, Neuroscience, and Immunology
CANCER BIOLOGY: PTEN expression is consistent in colorectal cancer primaries and metastases and associates with patient survival. Atreya, C.E. et al. (Warren). Cancer Medicine. 2(4):496-506.
Every cancer is unique. As a hypothetical scenario, take 10 individual diagnoses of colorectal cancer, and you’ll see 10 very different courses of the disease: Some may be rapidly lethal despite aggressive treatment, some may initially respond but ultimately become lethal, others may regress after only aggressive treatment, and some may regress easily. This kind of variation makes it extremely difficult to decide upon treatment options and often leaves patients with diminished confidence about their future.
How can we better identify how each cancer will behave? Increasingly, the answer seems to lie in genetics. In this paper, researchers sought to find a robust way of identifying more aggressive colorectal cancers by looking for the presence or absence of PTEN, a gene involved in regulating the cell cycle. They looked at tissue from primary or secondary metastases from a group of colorectal cancers and found around 10 percent had lost PTEN expression and validated this method for primary tumors (meaning that it works if you test it on the original tumors before they metastasize — that is, much earlier in the course of the disease). PTEN-deficient tumors were associated with an overall survival of nine months, as compared with 49 months for tumors that still had PTEN expression. PTEN expression can therefore be used as a way of determining the aggressiveness of colorectal cancer.
NEUROSCIENCE: Soluble guanylate cyclase generation of cGMP regulates migration of MGE neurons. Mandal, S.; Stanco, A.; Buys, E.S.; Enikolopov, G.; Rubenstein, J.L. Journal of Neuroscience. 33(43):16897-914.
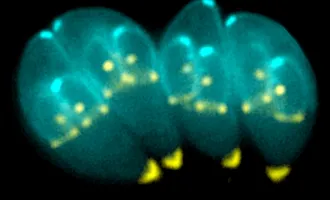
During brain development in the neocortex, neurons from a deep layer of the brain migrate upwards, then divide, causing a relative increase in the surface area of neurons at the top of the brain (neocortex) compared to the deeper layers of the brain. This surface area mismatch causes folding of the neocortex and the typical wrinkled appearance of our brains. During development, then, there is a lot of movement of neurons from deep in the brain to more superficial areas, so that this process can occur.
The medial ganglionic eminence (MGE) is one of those deep brain regions that neurons migrate through to get to the neocortex. In this paper, researchers wanted to identify the control mechanisms that govern neuron movement from the MGE into the neocortex. By using a panel of different mouse genetic knockouts that don’t have proper neuron migration for different genetic reasons, they were able to identify the common thread that causes defective neuron migration from the MGE. Nitric oxide-cyclic GMP is a circularized version of the nucleotide guanine bound to nitric oxide and is made by soluble guanylate cyclases extracellularly in the brain. Knockout mice for nitric oxide or guanylate cyclases had defective neuron migration from the MGE, indicating the importance of this molecule in neuron movement.
IMMUNOLOGY: Interaction of allergy history and antibodies to specific Varicella zoster virus proteins on glioma risk. Lee, S.T. et al. (Wiemels) International Journal of Cancer. October 11. [Epub ahead of print]
Gliomas, the most common type of brain or spinal cancer, present in highly diverse ways: Some are slow growing and don’t metastasize, while others can be extremely aggressive, metastatic and rapidly lethal. Gliomas are also poorly understood: Little is known about what causes them, and they can appear to strike patients at random. Significant effort has been devoted to identifying associations between glioma and unique exposures or other health conditions of glioma patients, in order to identify potential risk factors.
Interestingly, the presence of allergies and a history of chicken pox or shingles are negatively associated with the risk of glioma — meaning that people who have been infected with the varicella zoster virus and people with allergies have a lower risk of developing glioma. Here, scientists wanted to explore this potential relationship by testing glioma patients and healthy individuals for antibody responses to varicella zoster viral proteins. As compared with healthy individuals, glioma patients were found to have reduced antibody reactivity against the viral proteins. The healthy individuals were then separated into two further groups, low- and highly allergic individuals. Viral reactivity was associated with reduced glioma risk only in the highly allergic group. The authors conclude that the interaction between the allergic immune environment and specific antiviral antibodies may interact to help prevent gliomas.