The Reality of Brain Trauma in Sports
Recently, concern about the long-term effects of head trauma related to contact sports has skyrocketed. At the center of the controversy are the rising number of former football players suffering from a neurodegenerative condition and the National Football League (NFL), which has largely denied any link between football and degenerative disease.
Numerous stories have been written about the tragic deaths of former athletes, and Will Smith starred in a film about the forensic pathologist who first identified abnormalities in a former NFL player’s brain.
As media attention increases, the underlying biology is rarely the focus. Reporting is rarely neutral — any head injury is either a sure path to lifelong distress or there is no reason to believe any link at all exists. The reality, however, is murkier.
It is critical to assess what current research reveals, what still needs to be done, and why it is so difficult to make definitive claims.
The question is whether repeated head trauma causing minor brain injuries, such as concussions, can have effects later in life, particularly in the development of the neurodegenerative disease Chronic Traumatic Encephalopathy (CTE). Neurodegeneration associated with repeated head trauma had been described since the 1920s in boxers, but it was not until 2005 that the first case of CTE was diagnosed in an athlete from another sport.
CTE is a debilitating illness. Patients suffer from progressively worsening cognitive, emotional, and physical symptoms, including erratic moods, personality changes, and memory loss. However, these symptoms typically emerge about a decade after initial brain trauma, which makes it difficult to link earlier injury with an eventual CTE diagnosis.
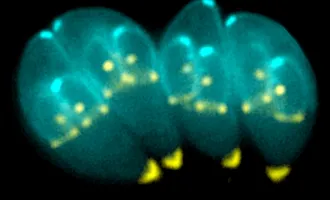
The only way to diagnose CTE is to examine brain tissue after death. Much like Alzheimer’s Disease, CTE causes abnormal buildups of a protein called tau. It is not known how these tau buildups are linked to the behavioral symptoms of CTE, but they are a key marker for diagnosis. Because postmortem analysis is the only way to diagnose CTE, several brain banks dedicated to CTE have been established.
At Boston University, one of the largest CTE brain banks, researchers have examined 165 total brains of former football players and found evidence of CTE in 97% of professional players and 79% of all players.
CTE has also been identified in athletes from other sports, including professional ice hockey and baseball. In a study from the Mayo Clinic, no evidence of CTE was found in 198 people with no history of playing contact sports or other head injuries.
Since CTE seems to occur overwhelmingly in people with a history of repeated minor head trauma, researchers have turned to initial head injuries to understand how CTE develops.
However, linking head trauma to CTE has proved scientifically difficult. Scientists currently think a concussion after a blow to the head causes minor traumatic brain injury, which induces changes in the brain leading to CTE. However, this link is difficult to investigate because concussive impacts and symptoms are heterogeneous, there are no clear diagnostic criteria for concussions, and we have a rudimentary understanding of the changes in the brain following a concussion.
Concussions are caused by forces applied to the brain due to sudden movements of the head. The brain is floating inside the skull in a bath of fluid that provides a buffer between the brain and skull. When sudden impact occurs and the head rapidly stops moving, the brain can continue to move, like when a person is thrown off a bicycle after a sudden stop. The brain can hit the inside of the skull, causing trauma.
There is not a known “impact threshold” where force to the head goes from benign to harmful. While it is possible to put sensors on helmets to detect the exact force exerted on the head during gameplay, this data has not yielded a clear threshold that could be used for diagnosis likely because other factors, including the angle of impact and individual susceptibility, affect concussive risk.
Not only is the threshold for an injury-causing impact unclear, the experiences of people with concussions are diverse. Symptoms include headaches, dizziness, fatigue, and memory impairment.
Contrary to popular belief, loss of consciousness is not required for a concussion. The variability of symptoms makes concussion diagnosis difficult, especially at the time of injury.
Standard sideline concussion tests assess coordination (walking in a straight line), memory (repeating a list of words), and other cognitive skills. However, these standard tests often perform poorly; in one study, a standard sideline test detected a concussion in only two of 12 athletes who were later diagnosed. Without a clear picture of causes or symptoms of concussions, identifying, treating, preventing, and researching concussions is difficult.
To understand how concussions lead to CTE, we must first understand the biology of concussions. The period immediately following initial injury is the best understood scientifically.
During normal function, the brain is precisely balanced. Immediately after concussion, the brain is hugely disrupted: there are large shifts in the normal ion balance and non-selective release of neurotransmitters, chemicals that neurons use to communicate with each other, causing a huge surge in random activity.
Following this massive disruption, neurons attempt to re-establish the proper balance in the environment. However, this rebalancing is extremely energetically demanding and often requires more resources than are available, particularly because blood flow providing nutrients and oxygen is also decreased after concussion. It can take weeks for the brain to recover, and during this time, the brain remains in a state of heightened vulnerability to further injury.
While there is some understanding of the chaos that a head injury immediately causes in the brain, scientists do not understand why symptoms persist in some patients much longer than in others or how these changes may cause CTE later in life.
There is a strong correlation between the amount of time someone is exposed to repeated head trauma — not the actual number of head injuries — and their likelihood of eventually being diagnosed with CTE, but scientists do not know how these traumas add up over the years.
Research into CTE is still in its infancy. One major problem is the small and potentially skewed sample of brains that have been donated to brain banks.
Diagnosing CTE requires a player or their family to elect to donate their brain to science. Therefore, it’s possible that brains with CTE are overrepresented in brain banks because only people with symptoms choose to donate.
One of the most famous CTE cases is that of Dave Duerson, a safety who played in the NFL for a decade.
Duerson sent a text message to his family requesting his brain be sent to Boston University before committing suicide. Duerson was experiencing extreme emotional and cognitive symptoms and thought CTE may have been to blame and was in fact diagnosed with CTE after a postmortem exam of his brain.
However, former athletes who feel healthy may not consider having their brains studied. While the Boston University team has found CTE in nearly all of the NFL players they have examined, this does not mean that all NFL players have CTE.
While CTE is certainly more common in people with a history of playing contact sports than in the general population, it may still only be a small fraction of those athletes.
Research is ongoing to both develop tests for diagnosis during the lifetime of former players, as well as attempts to recruit a broader range of people to donate their brains to brain banks.
Scientists and doctors continue to try to understand the link between concussions and CTE, but there is undoubtedly a strong correlation. Proving causation is often impossible in human studies, so correlation becomes the gold standard. Although research into CTE is ongoing, the results are already clear enough that the NFL’s denial of any links between head injury and subsequent neurodegeneration is irresponsible.
Additionally, an investigation from The New York Times showed that the NFL underreported head injury rates in their own data set of concussions in the NFL, making their statistics on the risk of head injury misleading and artificially low. The NFL does continue to conduct head injury research, but their history of misreporting data calls future conclusions into question.
Recently, Jeff Miller, the NFL Senior Vice President of health and safety policy, did say there was “certainly” a link between playing in the NFL and CTE, but others in the NFL later walked that statement back.
The path forward, both for current and former players, is unclear. Work is being done to reduce the impact of CTE by improving safety equipment to prevent concussions, refining sideline assessments to identify athletes at risk for lasting damage, and developing effective treatments for concussions.
Research is also being done into the development of CTE, including ways to diagnose and treat it during the lives of those who already have a history of head trauma.
The NFL can facilitate research by acknowledging the problem, but that is only the first step of many to better diagnose and treat those affected.