Finding the Fountain of Youth
For thousands of years, explorers, adventurers, and conquerors have searched for the “fountain of youth,” a magical spring that grants longevity to those who drink from it.
Today, the search continues, now led by explorers of a different kind — research scientists.
Although modern scientists use pipettes rather than compasses, the popular field of anti-aging research resembles the quest for the fountain in its obsessive motivation to increase lifespan.
The scientific practices in pursuit of this goal can be just as quixotic as the age-old attempts to locate the fountain.
Take Elizabeth Parrish: as CEO of biotech company BioViva, she is determined to stop aging and has not let the FDA or concerns for her own safety get in the way.
She flew to Colombia in September 2015 to test two gene therapy drugs on herself.
This experiment was not FDA approved because the drugs had not undergone the proper pre-clinical tests required to advance to human trials.
The drugs are intended to increase muscle mass and reverse the biological aging of cells by lengthening their telomeres1.
How Does It Work?
What are telomeres and why would Parrish want to make them longer?
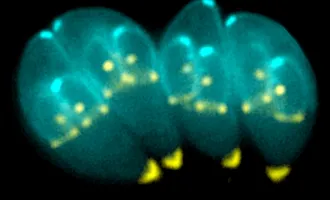
DNA, the molecular code that provides instructions for life, is coiled tightly in a rod-like shape, called a chromosome.
Telomeres are little caps of DNA on the ends of these chromosomes that are thought to be protective, preventing the chromosome from coming apart or fusing with other chromosomes.
Telomeres also serve a crucial function in DNA replication. During cell division, a process that creates healthy new cells to replace old or damaged cells, DNA must be replicated so the new cells can have a copy of the instructions for life.
However, the machinery involved in DNA replication can’t fully reach the end of the chromosome (think of a zipper — even when fully zipped, there are always a few teeth on the end that are not fully interlocked), so the copied chromosome is always a little bit smaller than the original.
Eventually, important information in the DNA can get lost, which can cause the newly-divided cells to become dysfunctional. To prevent this loss, telomeres act like extra teeth at the end of the zipper, sacrificing themselves so that all the important information from the chromosome can be copied.
The telomeres are replaced, but not quickly enough to keep up with the pace of cell division, so over time the ends of chromosomes become shorter.
Without telomeres, chromosomes start sticking to each other, mixing up DNA, and new cells lose information with every division.
This makes it very hard for the new cells to function properly — imagine trying to cook from a recipe book where everything is out of order and some pages have been ripped out.
Telomere shortening has been observed in aging and aging-related diseases. Some researchers think it is just a byproduct of aging, like getting gray hair, while others think it is the cause of age-related health problems.
The people at BioViva are in the latter camp. Their solution is to prevent telomere shortening or to artificially lengthen them, which they think will reverse or slow the aging process.
Fountain of Youth Achieved?
Were the BioViva drugs effective at lengthening Elizabeth Parrish’s telomeres? BioViva claims that the telomeres in Parrish’s white blood cells lengthened by 9% just six months after treatment, but many scientists are skeptical of the scientific rigor with which these tests were conducted.
Some have pointed out that this difference of 9% falls within the measurement error of most research laboratories and is too close to the variance of most telomere length assays to be convincing.
Even if the drug is as effective as claimed, there are a number of ethical and safety considerations that accompany this experiment, and BioViva’s drugs will still need to undergo the proper regulatory steps before being considered for FDA approval.
Traveling abroad to sidestep U.S. preclinical requirements does not accelerate this process.
In a field racing against time, Parrish seems to be wasting it.
Furthermore, as a for-profit company, having the CEO test a potential therapy on herself also reflects a conflict of interest, because one of their primary objectives is to make a profit by getting products on the market as quickly as possible, which could influence how much Parrish is willing to put her health and others’ at risk.
People have rushed drugs into clinical trials before, only to encounter terrible outcomes.
In the late 1990s, Jesse Gelsinger, a young man living with a metabolic disorder, entered a clinical trial of a new gene therapy for the disorder.
He experienced an unexpected and fatally severe immune response to the treatment.
His death sparked an FDA investigation; the resulting clinical trial regulations require full disclosure of information about any potential health problems.
BioViva has not reported any harmful side effects of Parrish’s treatment thus far, but having performed the procedure outside of the U.S., they are not legally required to do so.
Even if Parrish is not adversely affected by the drug, that doesn’t mean that others won’t be; a much larger sample is required to conclude that a drug is safe.
How to Approach Testing?
Testing these drugs in another country in order to shirk safety and transparency measures is a refusal to learn from the past and is irresponsible and disrespectful.
Bioviva’s approach to anti-aging, that is, manipulating DNA, is not the only avenue of unconventional anti-aging research — another example is parabiosis.
This long-used technique involves sewing together two animals, typically rodents, so they share a circulatory system.
Scientists can investigate how factors that circulate in the bloodstream of one animal affect the other animal.
In aging studies, where an old mouse and a young mouse are connected, young blood promotes the formation of new neurons and more cell division in different tissues, suggesting that something in the blood is restoring the old mouse to a more youthful condition.
Although access to the younger animal’s blood does not increase the older mouse’s lifespan4, these results suggest that transfusions of youthful blood could reduce the likelihood of developing age-related diseases and improve the quality of later years of life.
Like gene therapy, blood transfusions are just beginning to enter clinical trials in humans for treating diseases such as Alzheimer’s, but they are also accompanied by many questions and risks.
For instance, it’s not clear that the effects of a single transfusion would last long enough to have a meaningful impact on a person’s health, and there are concerns that repeated blood transfusions might over-activate stem cells, leading to aberrant cell division and possibly cancer.
Treat Age, Prevent Disease
Regardless of the kind of intervention, the future of anti-aging research relies heavily on the opinion of the FDA.
Currently, the FDA does not consider aging in and of itself to be a disease, so any drug seeking approval must be directed toward a specific aging-related condition.
The primary reason for this classification is that aging is a natural and universal process, unlike diseases, which are characterized as deviations from “normal”.
A counterargument gaining traction is that treating aging may have broader effects on health outcomes than treating specific age-related diseases, because this strategy may prevent diseases or delay their onset.
A team of researchers is hoping to prove this point and change the FDA’s position with a clinical trial called Targeting Aging with Metformin, or TAME.
The drug, metformin, will be given to people who have a subset of age-related conditions: cancer, heart disease, or cognitive impairment.
Participants will be monitored to see whether TAME protects them from developing the conditions they don’t already have and/or extends their lifespan5.
The FDA is currently deciding whether to allow this trial, but if they do so and if metformin successfully prevents the development of age-related diseases, it may pave the way for more funding and recognition of aging as a treatable condition.
Considering that aging is accompanied by a biological decline in physical and mental capabilities, and is one of the greatest risk factors for human disease3, it’s no surprise that a hefty number of resources are funneled into studying causes and cures for aging.
But whether or not the FDA reclassifies aging as a disease, the current clinical applications of aging research should focus more on improving the quality of life over a typical lifespan rather than extending life itself.
The motivations behind experiments intended to extend lifespan are controversial, and also fail to take into account another important issue: as a society, we have not yet taken the time to thoroughly analyze the societal, economic, and financial consequences of extending human life.
Scientists, clinicians, drug companies, policymakers, and others must work together to consider all the risks and possible outcomes and figure out how to support a population that is living longer.
In the meantime, the fascinating aging studies that are performed in animal models should be translated to human studies in an ethical and responsible manner, which means taking a little more time to go through the proper regulatory channels.
Unfortunately for the impatient, time is exactly what anti-aging research is trying to fight.