Change Your Breathing—Now!
Recently I attended the Anesthesia Grand Rounds’ “Updates in Pain Management.” (Yes—we physical therapy students are involved!) The event featured many well-known practitioners, and a psychologist in particular brought my attention back to the diaphragm. C3, C4, C5 keep the diaphragm alive, may be where some individuals’ knowledge of the diaphragm starts and ends—but not for UCSF students!
Diaphragm 101
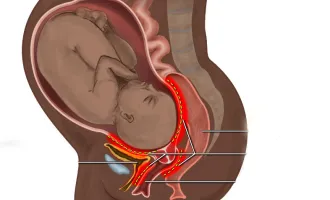
A quick refresher on diaphragm anatomy: the diaphragm is a dome-shaped muscle, located just below the ribcage, whose fibers from the xiphoid process, vertebrae and ribcage converge into a central tendon. The diaphragm is innervated by the phrenic nerve, and when it contracts, its fibers shorten, move inferiorly and allow air to be drawn into the chest cavity.
Non-respiratory-related, the diaphragm works surprisingly well to eject less-than-glamorous bodily fluids. Often overlooked, the diaphragm also has an intimate relationship with the pelvic floor. As the diaphragm descends and contracts during inspiration, the pelvic floor also lowers but extends, and during exhalation the diaphragm lengthens upward while the pelvic floor elevates and contracts slightly. In other words, the diaphragm is deeply integrated into the core system, whose other components include the transversus abdominis anteriorly and multifidi posteriorly.
Belly Breathing
Diaphragmatic breathing, aka abdominal breathing, has been shown to reduce stress, likely due to slowing respiratory rate and heart rate, and activating the parasympathetic nervous system. It has also been touted that abdominal breathing strengthens the diaphragm, decreases oxygen demand and decreases the effort required to breathe.
How to Do It
The psychologist from Grand Rounds referenced Dr. Weil’s “Relaxing Breath” exercise, which Dr. Weil cites as a “natural tranquilizer” that can be done anywhere. To do the exercise, either lie on your back with your knees bent or sit up straight in a chair, then place one hand on your sternum and the other on your abdomen. After a complete exhalation, inhale quietly through your nose for four seconds, hold the breath for seven seconds and exhale completely through your mouth for eight seconds (“whoosh” sounds encouraged!).
As you inhale, let your belly push against your bottom hand, and you should feel little movement at your top hand. The point is to maximize the diaphragm’s role in breathing, and minimize the use of accessory muscles. According to Dr. Weill, you cannot do this exercise too much, and he recommends starting with four breaths, twice a day.
The Take Home
Diaphragmatic breathing is easy to perform and teach, and can be recommended by any health care practitioner. It may significantly help your patients with chronic pain—so give it a try!
Side note: Diaphragmatic breathing may not be recommended for all patient populations. There is some suggestion that diaphragmatic breathing may reduce efficiency of breathing in individuals with moderate to severe COPD. So use your clinical judgment!