Using the Body to Fight Cancer
In the fight against cancer, harnessing the natural defense mechanisms within the human body is gaining promise.
Termed cancer immunotherapy, researchers have discovered ways to bolster the immune system to recognize and kill cancer cells.
The immune system is a network of cells, tissues, and organs that responds to and removes foreign invaders introduced to the body.
Cancer cells originate from normal cells in the body, making it difficult for the immune system to naturally recognize them as foreign.
Additionally, cancer cells develop defense mechanisms against the immune system, secreting factors that suppress immune response, and even altering immune cells to support tumor growth.
Immunotherapy is designed to re-awaken the immune system by blocking these suppression signals and engineering cancer specific recognition.
Matthew Spitzer, a Sandler Fellow here at UCSF, is leading research directed at how the system-wide immune response changes in response to cancer, and how this information can be used to improve immunotherapy.
His lab more broadly focuses on how the immune system is poised to make decisions, to attack or not to attack, based on the environment or prior experiences of an organism.
“[The immune system in cancer] seems to be one of these really interesting settings in my mind, where one biological system can approach the same fundamental problem and make a very different decision about how to respond to it,” he said.
The UCSF Sandler Fellows Program supports recently graduated PhDs or MDs in establishing independent research laboratories, bringing in energetic and creative minds to investigate challenging biomedical questions.
Spitzer was inspired to be a principle investigator by “the combination of the intellectual freedom you have to pursue the ideas that you think are interesting, and working with peers and colleagues that are equally motivated to advance the science of biology and disease.”
Though collaboration between Stanford University and UCSF, Spitzer published an article in Cell last week demonstrating that effective cancer immunotherapy requires coordinated changes across the immune system, not just within the tumor itself.
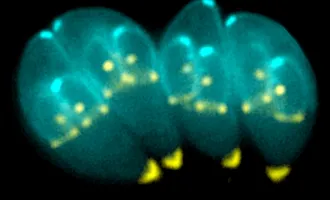
He uses a new technology, called Mass Cytometry, to model system-wide immune response.
Mass cytometry, or CyTOF, is a new technology developed by Scott Tanner at the University of Toronto, and first tested scientifically in Garry Nolan’s lab at Stanford.
CyTOF allows researchers to simultaneously measure the expression of up to 40 proteins, or protein activity states, in single cells.
Proteins are the molecules in cells that execute the majority of biological functions, from sensing the environment and communication between cells, to cellular metabolism and division.
This technology is an advance on flow cytometry, which uses fluorescent markers to label up to 16 proteins in single cells.
Flow cytometry is limited by the detectable wavelengths of light. There are only so many colors of light the machine can detect.
Another challenge is distinguishing between the different wavelengths of light, because they overlap.
Mass cytometry overcomes the limitations of flow cytometry by using different masses to tag a protein, instead of light emission.
Looking at the periodic table, each element has a different atomic mass unit, or weight at the scale of a single molecule.
Mass spectrometers are machines that can determine the mass of a molecule by its time of flight, or how fast it moves through the machine. Heavier particles move slower than smaller ones.
Different masses are easier to distinguish than different wavelengths of light, making the results more clear and convincing.
Analyzing protein expression in single cells is important because individual cells vary quite a bit from one another.
Researchers are beginning to appreciate critical differences between single cells that affect the decisions they make when they encounter changes in their environment.
Spitzer pioneered the use of CyTOF to study global immune dynamics in animal models of disease, allowing his to ask fundamental scientific questions.
He uses the 40 different mass labels to identify distinct immune cell populations, and measure their abundance and activity under different conditions.
Spitzer believes that understanding the immune response at the level of the whole system, while appreciating differences between individual cells, is most informative in understanding how cancer influences immunology.
“We can start to paint a much more comprehensive picture of how a tissue system is behaving or how it’s responding to some sort of change in the physiology of the organism,” he said.
In his latest publication, “Systemic Immunity Is Required for Effective Cancer Immunotherapy,“ Spitzer uses a mouse model of breast cancer to compare how the immune system changes in response to ineffective or effective immunotherapy.
His findings challenge two widely accepted beliefs in the field of cancer immunology: immune cells within the tumor are responsible for anti-tumor response, and immune cells with killing functions (cytotoxic CD8 T cells) are the most critical cell type.
In Edgar Engelman’s Lab at Stanford, Spitzer was previously involved in the development of a new effective immunotherapy against breast cancer.
This therapy combines cancer targeting, using tumor-binding antibodies, and immune cell activation, by stimulating an immune cell receptor called CD40 and adding a signaling molecule called interferon γ.
To understand what distinguishes an immune system capable of coordinating an effective response against cancer, Spizter compared this effective treatment in mice against an immunotherapy previously found to be ineffective in breast cancer.
Spizter analyzed immune cell populations in the tumor, but also in a variety of lymphoid organs across the body, or locations where immune cells develop and mature.
These include the nearest lymph node, the blood, and even distant immune organs like the bone marrow and spleen where immune cells develop and are primed for attack.
He studied two time points after treatment with immunotherapy: initial activation of immune response, the initiation phase, and effective immune attack on tumor cells, the rejection phase.
By identifying which cell populations were expressing a marker of cell division, Ki67, Spizter demonstrated that immune cells expand in the peripheral immune system (outside the tumor) and within the tumor during the initiation phase.
However, during the rejection phase, when the tumor is being killed, immune cells are only expanding in the periphery.
This means that immune cells attacking the tumor are being generated outside of the tumor.
Next, the researchers asked whether immune cells created in the periphery were necessary for tumor eradication.
They treated mice with a molecule that blocks immune cell migration from the periphery to the tumor, FTY720, and found that the effective immunotherapy now failed to kill tumors.
Instead, tumors continued to grow.
“Our studies showed that when an immune response was being initiated by an effective immunotherapy, it was required that immune cells outside of the tumor be primed, that new immune responses be formed,” said Spizter.
The second dogma challenged in this publication is that CD8 cytotoxic T cells are the most important immune cell type in cancer immunotherapy, the cells actually responsible for invading and killing the tumor.
CD4 T cells are immune support cells, important for coordinating immune responses and activating cells like CD8 T cells.
Spizter found that CD4 T cells were highly increased during an effective immune response against cancer.
He collected CD4 T cells from the blood of mice that received effective immunotherapy against the breast cancer model, and transferred them into to a new tumor-baring mouse that received no therapy.
The new mouse was able to mount an effective immune response that killed the tumor.
In an exciting collaboration with Lawrence Fong at UCSF, they were able to confirm that CD4 T cells were also significantly increased in the blood of human cancer patients that were responding well to immunotherapeutic drugs.
“This really suggested that we had identified something really important,” said Spizter.
Through the use of an inclusive, system-wide approach to studying the immune system in cancer, Spizter and colleagues were able to uncover novel principles of effective versus ineffective immune response.
Spizter hopes that his findings will broaden the scope by which people characterize the immune system, and to think about sites outside of the tumor that may be important.
While cancer immunotherapy is growing as a practice, it has only been effective in a small subset of patients.
In speculating on the future of the field of cancer immunology, Spizter cited the growing number of cancer drugs being developed.
“[We need] a robust enough understanding of the immunological mechanisms that mediate anti-tumor immunity, such that we can rationally understand what combination of perturbations should be made in a particular patient to maximize their probability of success,” he said.
Look out for more discoveries in systemic immunology by the Spitzer lab at UCSF.