Journal Club: Cancer Biology/Microenvironment
Presentation: “Resistance Is Only ‘Skin’ Deep: Dissecting the interactions between tumor cells and their micro-environment in melanoma”
Presenter: Bianca Lee (second-year BMS student)
Paper: Straussman R, et al. Tumour micro-environment elicits innate resistance to RAF inhibitors through HGF secretion. Nature. 2012 Jul 26;487(7408):500-4.
In a nutshell:
One of the major challenges in cancer treatment is the development of drug resistance. Even when patients initially respond to chemotherapy, tumors often recur because they have mechanisms to evade complete elimination by the drugs. A few cancer cells might have acquired mutations that allow them to survive drug exposure, and these surviving cells can develop into another tumor. Another possibility that the authors of this paper investigate is resistance conferred by the tumor microenvironment. It’s a question of nature versus nurture on a cellular level.
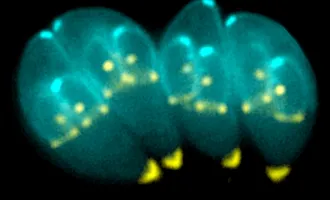
In recent decades, scientists have become aware of the important role of the microenvironment. This includes the normal cells (researchers often talk about stromal cells, which comprise the connective framework around an organ or tumor) and the factors they secrete, which can influence tumor growth and metastasis.
First, the authors used a co-culture system to figure out if stromal cells could confer drug resistance. They found that many potent drugs that could kill cancer cells cultured alone were no longer able to do so when the cancer cells were cultured with stromal cells, indicating that the stroma is indeed important in conferring resistance.
How do they do that? Specifically, is it cell-cell contact or a secreted factor? The authors focused on BRAF-mutant melanoma, which has a high rate of resistance to the RAF inhibitor vemurafenib. They found that fibroblast-conditioned medium was able to rescue cancer cells from the drug and concluded that fibroblasts secreted a factor that conferred resistance.
They identified this factor as hepatocyte growth factor (HGF), which signals through well-established growth pathways such as PI3K/Akt and Ras/Raf. Indeed, the authors confirmed that HGF is both necessary and sufficient for the stroma-mediated rescue of cancer cells.
When they depleted HGF, the cancer cells died, and they could rescue them by adding HGF back. They further investigated the mechanism by which HGF confers resistance and determined that it does so by restoring growth-promoting factors such as pERK and Akt.
The identification of HGF and its downstream pathway reveals a new drug target and points to a possible combinational therapy—perhaps BRAF-mutant melanomas can be more effectively battled by combining a RAF inhibitor with an Akt inhibitor to prevent or delay drug resistance. Ultimately, the authors identified a new mechanism by which cancer cells develop drug resistance, one that implicates the microenvironment surrounding tumors, and they uncovered a possible therapeutic technique.